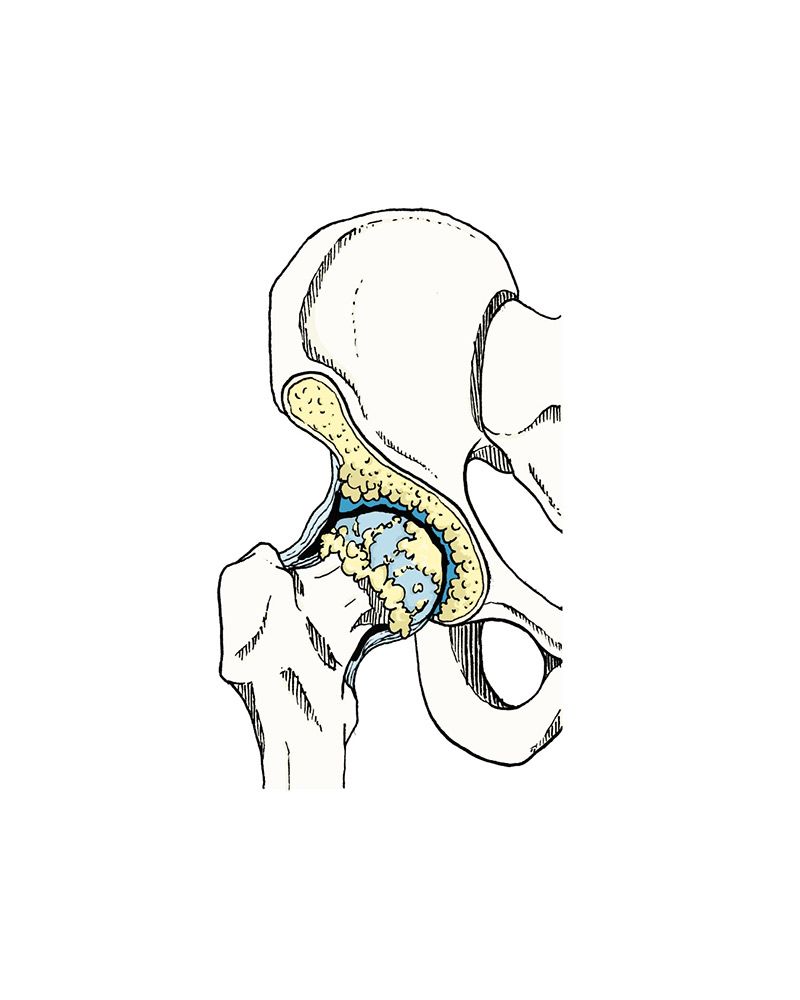
Coxarthrosis, osteoarthrosis or arthrosis of the hip is nothing more than the progressive wearing away and disappearance of the noble tissue that constitutes the hip joint, which is the cartilage.
Coxarthrosis / Hip arthrosis
The causes can be primary or idiopathic and secondary. Secondary causes may be post-traumatic (fracture, fracture sequelae or repeated trauma), post femoral-acetabular impingement, post-infectious (septic arthritis), as a result of joint or systemic medical disease (ankylosing spondylitis, rheumatoid arthritis, diabetes mellitus, avascular necrosis of the femoral head, among others), post-dysplastic hip disease (change in the anatomy of the joint) or other childhood hip diseases such as Perthes’ disease.
The pain is typically localized on the anterior surface of the hip (groin). It may extend to the knee (sometimes confused with knee pain) or to the gluteal region (buttock) and may be confused with pathology of the lumbar spine. The pain worsens when the lower limb rotates (crossing the leg). In parallel, it is often accompanied by a progressive loss of mobility characterised by the inability to put on shoes and/or socks or clip nails.
The examination required for diagnosis is a simple X-ray of the hip and pelvis. Other tests are not necessary for a correct diagnosis, but it may be necessary to use magnetic resonance for a more detailed joint study or computerised tomography in cases of arthrosis involving large deformities or bone tumours.
In the initial phase, treatment aims to control pain and prevent the progression of the disease. It is based on the use of analgesics, anti-inflammatories and chondroprotectors (glucosamine and chondroitin). Conventional physiotherapy resources play their part in this pathology and aim not only to aid the process of pain control through physical agents, but also to improve the muscular envelope around the joint. Exercises such as Pilates, water aerobics and cycling are often recommended. Joint infiltrations (anti-inflammatories; viscosupplementation or growth factors) can be done with the aim of improving pain in cases where oral medication is not effective.
The vast majority of cases, depending on the degree of arthrosis, improve their symptoms with 2 to 3 weeks of treatment with an analgesic and an anti-inflammatory. Taking chondroprotectors may improve the complaints, but only after 3 to 6 months use. Joint infiltrations may improve complaints for a period of 6 months to 1 year, and may be repeated at the end of this time.
When these treatment methods are no longer effective, surgical intervention may be necessary to replace the diseased joint with a hip prosthesis (total hip arthroplasty). The recovery time for a hip replacement varies according to age, physical ability and the surgical technique used. In an active patient who has undergone anterior total hip replacement, recovery time is around 2 to 4 months.